Mako Total Knee
Mako for Total Knee replacement
We understand that knowing what to expect from your joint replacement experience is important to you. As you are reading through this material, please reach out to us to discuss if you have additional questions.
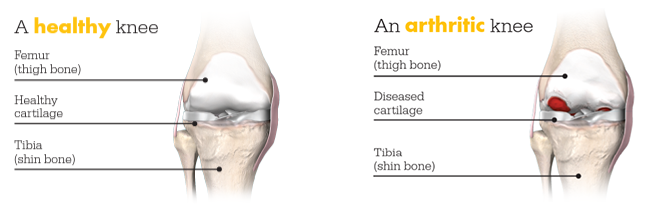
Each patient is unique and can experience joint pain for different reasons. It’s important to talk to us about the reason for your knee pain so you can understand the treatment options available to you. Pain from arthritis and joint degeneration can be constant or come and go, occur with movement or after a period of rest, or be located in one spot or many parts of the body. It is common for patients to try medication and other conservative treatments to treat their knee pain. If you haven’t experienced adequate relief with those treatment options, you may be a candidate for Mako Total Knee replacement, which may provide you with relief from your knee pain.
Mako can help your surgeon plan for better outcomes, like less pain and shorter recovery times, compared to manual knee replacement surgery.1
How Mako Works
Mako is an innovative solution for many suffering from painful arthritis of the knee.
Scan. It all starts with a CT scan so your surgeon can know more about your anatomy.
Plan. The CT scan is used to create a 3D CT-based model of your knee. Your surgeon uses this 3D model to create a personalized surgical plan and assist your surgeon in performing your knee replacement procedure.
Mako Can. In the operating room, your surgeon follows your personalized surgical plan while preparing the bone for the implant. The surgeon guides Mako’s robotic arm within the predefined area, and Mako’s AccuStopTM technology helps the surgeon stay within the planned boundaries that were defined in the personalized surgical plan to prepare the bone for the Triathlon Total Knee implant. With over a decade of clinical history, Triathlon knee implants are different from traditional knee replacement implants because they are designed to work with the body to promote natural-like circular motion.2-5

It’s important to understand that the surgery is performed by an orthopaedic surgeon, who guides Mako’s robotic arm during the surgery to position the implant in the knee joint. Mako does not perform surgery, make decisions on its own or move without the surgeon guiding it. Mako also allows your surgeon to make adjustments to your plan during surgery as needed.
IMPORTANT INFORMATION
Total knee replacement
Knee replacement is intended for use in individuals with joint disease resulting from degenerative and rheumatoid arthritis, or avascular necrosis.
Knee joint replacement is intended for use in individuals with joint disease resulting from degenerative, rheumatoid and post- traumatic arthritis, and for moderate deformity of the knee.
Joint replacement surgery is not appropriate for patients with certain types of infections, any mental or neuromuscular disorder which would create an unacceptable risk of prosthesis instability, prosthesis fixation failure or complications in postoperative care, compromised bone stock, skeletal immaturity, severe instability of the joint, or excessive body weight.
Like any surgery, joint replacement surgery has serious risks which include, but are not limited to, pain, infection, bone fracture, change in the treated leg length (hip), joint stiffness, hip joint fusion, amputation, peripheral neuropathies (nerve damage), circulatory compromise (including deep vein thrombosis (blood clots in the legs)), genitourinary disorders (including kidney failure), gastrointestinal disorders (including paralytic ileus (loss of intestinal digestive movement)), vascular disorders (including thrombus (blood clots), blood loss, or changes in blood pressure or heart rhythm), bronchopulmonary disorders (including emboli, stroke or pneumonia), heart attack, and death.
Implant related risks which may lead to a revision of the implant include dislocation, loosening, fracture, nerve damage, heterotopic bone formation (abnormal bone growth in tissue), wear of the implant, metal and/or foreign body sensitivity, soft tissue imbalance, osteolysis (localized progressive bone loss), audible sounds during motion, reaction to particle debris , and reaction to metal ions (ALTR). Hip and knee implants may not provide the same feel or performance characteristics experienced with a normal healthy joint.
The information presented is for educational purposes only. Speak to your doctor to decide if joint replacement surgery is appropriate for you. Individual results vary and not all patients will return to the same activity level. The lifetime of any joint replacement is limited and depends on several factors like patient weight and activity level. Your doctor will counsel you about strategies to potentially prolong the lifetime of the device, including avoiding high-impact activities, such as running, as well as maintaining a healthy weight. It is important to closely follow your doctor’s instructions regarding post-surgery activity, treatment and follow-up care. Ask your doctor if a joint replacement is right for you.
Stryker Corporation or its other divisions or other corporate affiliated entities own, use or have applied for the following trademarks or service marks: AccuStop, Mako, Triathlon. All other trademarks are trademarks of their respective owners.
References- B. Kayani, S. Konan, J. Tahmassebi, J. R. T. Pietrzak, F. S. Haddad Robotic-arm assisted total knee arthroplasty is associated with improved early functional recovery and reduced time to hospital discharge compared with conventional jig-based total knee arthroplasty: A PROSPECTIVE COHORT STUDY Bone and Joint Journal: 2018; 100-B:930–7.
- Mistry JB, Elmallah RK, Chughtai M, Oktem M, Harwin SF, Mont MA. Long-term survivorship and clinical outcomes of a single radius total knee arthroplasty. Surg Technol Int. 2016;28:247-251.
- Piazza S. Designed to maintain collateral ligament stability throughout the range of motion. Stryker-Initiated Dynamic Computer Simulations of Passive ROM and Oxford Rig Test. 2003.
- Wang H, Simpson KJ, Ferrara MS, Chamnongkich S, Kinsey T, Mahoney OM. Biomechanical differences exhibited during sit-to-stand between total knee arthroplasty designs of varying radii. J Arthroplasty. 2006;21(8):1193-1199. doi:10.1016/j.arth.2006.02.172
- Gómez-Barrena E, Fernandez-García C, Fernandez-Bravo A, Cutillas-Ruiz R, Bermejo-Fernandez G. Functional performance with a single-radius femoral design total knee arthroplasty. Clin Orthop Relat Res. 2010;468(5):1214-1220. doi:10.1007/s11999-009-1190-2
JR-MKOSYM-OTHW-747688
Copyright © 2023 Stryker